Navigating the Menopause Maze: Insights and Innovations
Menopause Decoded – A Comprehensive Guide
Menopause is more than just the end of menstruation; it's a significant phase in a woman's life that brings various changes and challenges. While the average age of menopause is between 51 and 52, it can occur anytime from the early 40s to late 50s. In this guide, we'll delve into what menopause entails, its symptoms, and the latest treatment options, offering clarity and confidence for those navigating this transition.

Understanding Menopause Symptoms
Menopause marks the end of a woman's reproductive years, occurring when the ovaries run out of eggs. The transition, known as perimenopause, can last one to two years, with symptoms like irregular periods, hot flashes, and mood changes.
Symptoms and Concerns
The hallmark of menopause is hot flashes, experienced by almost all women. These can vary in intensity and frequency, often worsening at night and disrupting sleep. Other common symptoms include night sweats, mood changes, decreased libido, accelerated bone loss, and vaginal dryness.
Hormonal Therapy and Alternatives
Hormonal therapy, a traditional menopause treatment, faced scrutiny after the early 2000s WHI study, particularly regarding Premarin and Provera. This led to a reevaluation of hormone therapy, highlighting the need for safer alternatives. Today, treatments like bioidentical hormones Estradiol and micronized progesterone offer effective relief with a favorable risk-benefit profile.
Long-Term Management
The decision to start hormonal therapy is personal and should consider individual health profiles. Most women can continue hormonal therapy indefinitely, enjoying benefits like improved sleep and stronger bones. Misconceptions about bioidentical hormones often arise, but at Herrmann Practice, we provide clear, factual information to guide our patients.
Special Considerations
Menopause's onset can be unpredictable, and in some cases, it may occur prematurely before the age of 40 due to factors like autoimmune processes or chemotherapy. Additionally, surgically removing both ovaries also induces menopause. Understanding these nuances is key to personalized menopause care.
Find out more about menopause and how the Herrmann Practice can help you through menopause
here.

The Truth About Bioidentical Hormones
Bioidentical hormones, often surrounded by misconceptions, are as effective and natural as any other hormone products. Estradiol, for example, can be applied through the skin, offering a safer alternative to oral pills by minimizing blood clot risks.
Bioidentical Hormones Explained:
Bioidentical hormones like Estradiol and micronized progesterone are FDA-approved and offer a safe, effective treatment for menopause symptoms. They are as 'bioidentical' as any hormones available on the market.
Addressing Concerns:
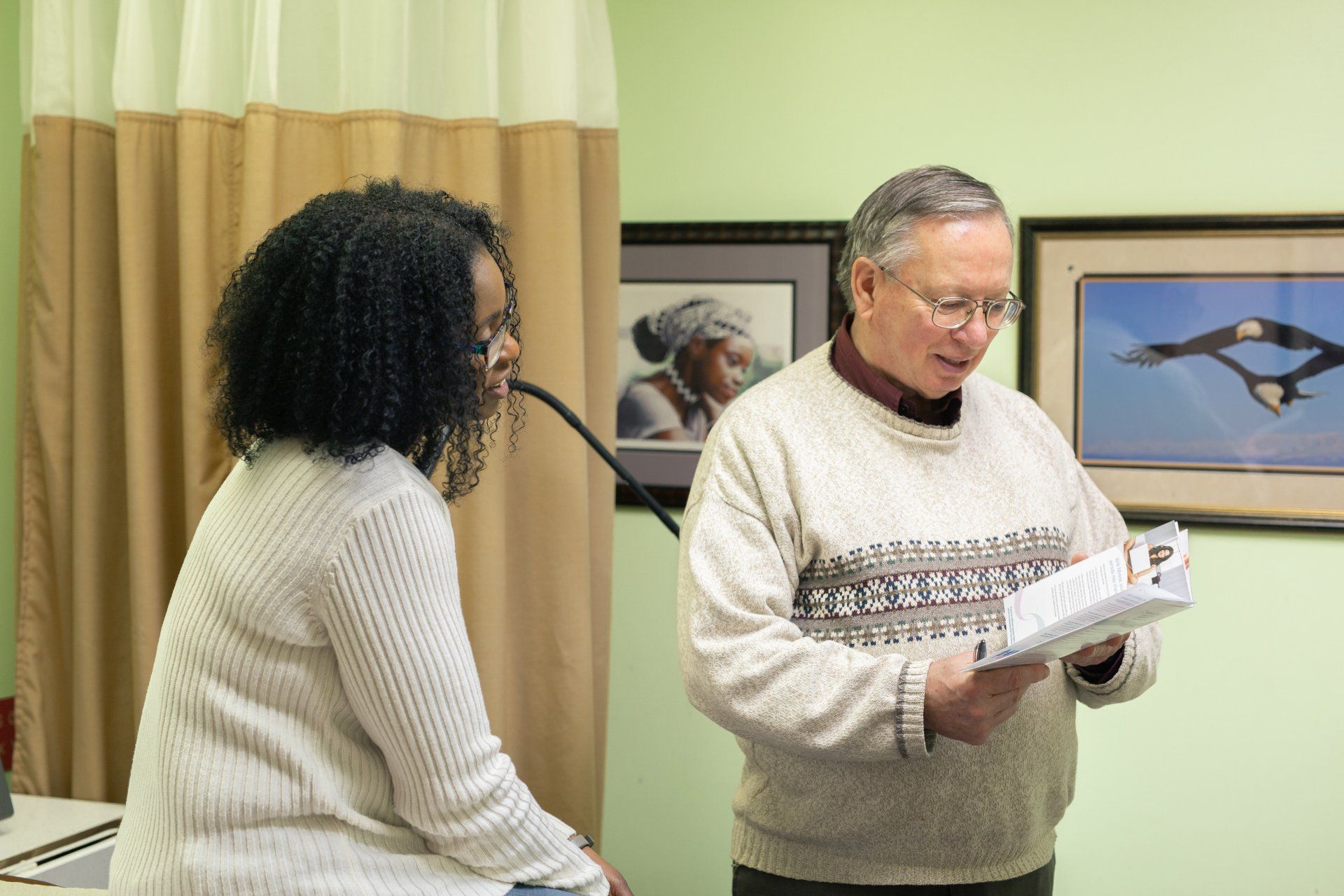
Patients often have concerns about the safety and efficacy of hormonal treatments. At Herrmann Practice, we address these concerns by providing up-to-date information and personalized treatment plans.
Charting Your Path Through Menopause
Navigating menopause requires understanding, support, and the right medical guidance. At Herrmann Practice, we're dedicated to providing comprehensive care and the latest treatment options for menopause. Whether you're beginning to notice the signs of perimenopause or are seeking ways to manage post-menopausal health, we're here to support and guide you through this significant life transition.
Ready to navigate your menopause journey with confidence?
Book an appointment with our experts at Herrmann Practice today. Embrace this phase of life with the knowledge and care you deserve.