The A to Z on HSV and HPV
The A to Z on HSV and HPV

Beyond the Acronyms –
Your Health Unveiled
Ever mixed up HSV and HPV? You're not alone. These acronyms pop up often in women's health discussions, but they represent very different health concerns. While both are viruses that affect millions, their impacts, treatments, and preventions vary. In this guide, we'll decode these terms, shedding light on their significance and offering clarity for better health decisions.
HSV: More Than Just Cold Sores
Herpes Simplex Virus, or HSV, is a prevalent virus with two distinct types: HSV-1 and HSV-2.
HSV-1: Often the culprit behind cold sores, it affects nearly half of the U.S. population over 50.
HSV-2: This sexually transmitted variant leads to genital lesions, impacting about 12% of the U.S. populace.
Many infected individuals remain symptom-free. Both types can lie dormant, reactivating when the immune system is weakened.
Symptoms and Concerns:
Many individuals infected with HSV may never show symptoms. Both types can lie dormant in the nervous system, becoming active when the immune system is weakened. HSV-2 is particularly distressing due to its social implications and the risk of transmission to sexual partners.
Treatment and Testing:
HSV can lead to painful open sores, with the initial infection often being the most severe. Medications are available to reduce the severity and frequency of outbreaks, but they cannot eradicate the virus. The primary medical concern arises if a pregnant woman has an active infection during delivery, as this can lead to severe infections in the newborn. In most cases, a C-section can prevent this transmission.
Common Queries:
A frequent question posed by patients is the duration they've had the virus before symptoms appear. This varies as everyone's immune system responds differently. Testing is most effective during an active outbreak, with a swab of the lesion detecting the virus. Blood tests, which detect herpes antibodies, indicate exposure but not necessarily an active infection.

HPV –
The Silent Threat to Women's Health
HPV, or Human Papilloma Virus, is the main cause of cervical cancer. It's notably prevalent among sexually active women under 30, with some estimates as high as 80%.
Treatment and Prevention:
While there's no specific medication for HPV, the Gardasil vaccine offers a shield of protection. It's crucial to get vaccinated before exposure. Most patients' immune systems will eliminate the HPV virus by age 30.
Testing and Prevalence:
HPV can be detected on a pap smear. However, due to its high prevalence among women under 30, routine testing isn't standard for this age group.
Vaccination:
The Gardasil vaccine protects against strains of HPV that cause cervical cancer and genital warts. Pediatricians recommend the vaccine for both boys and girls starting at age 9. A common question is the rationale behind such early vaccination. The answer lies in the enhanced immune response in younger children. Before age 15, only two doses are required. The primary side effect is soreness at the injection site, but it's a small price to pay for a vaccine that can prevent cancer.
Knowledge is Power
in Women's Health
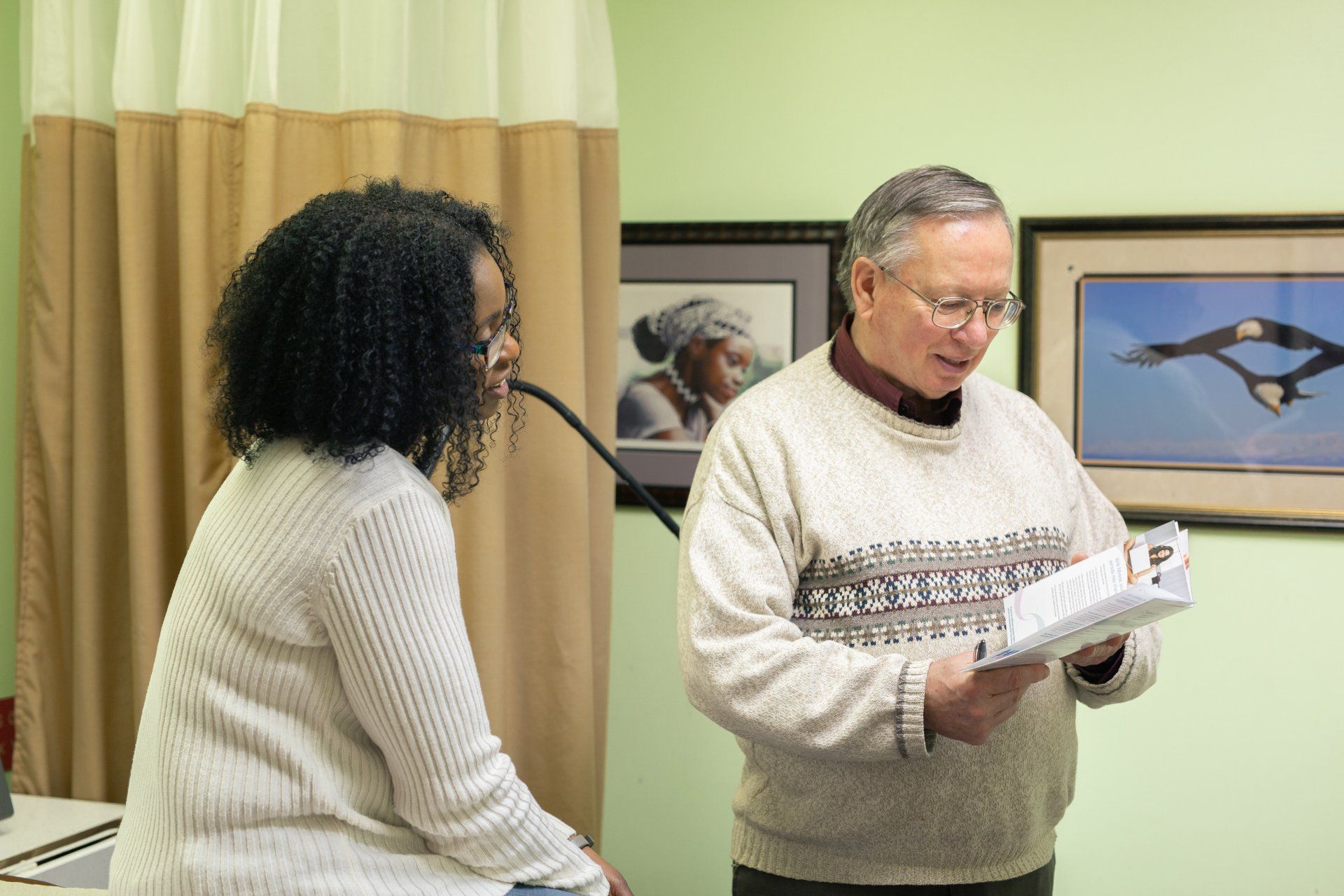
Grasping the intricacies of HSV and HPV is a step towards empowered health decisions. We're dedicated to providing you with trusted, compassionate healthcare insights. Questions or concerns about your health? Don't hesitate. Book an appointment with our experts at Herrmann Practice today. Prioritize your health; we're here to guide you.